Police throughout the nation have intensive training before becoming officers. That is as it should be for such a complicated job. What is not very well known is most locals only provide 4 hours of training on encountering the mentally ill.
Mental Illness is such a complex human condition that psychiatrist go three additional years after medical school. The lack of baseline training provided regarding mental illness, is a very discouraging fact, and an unfair allocation of training priorities to police officers. An encounter with a symptomatic person is a challenge with most times a good result. These situations can also get out of control in an instant resulting in outcomes such as arrests, beatings and sometimes death. Prior to 1988 the norm was for the family and advocates to get outraged, the press to focus on the incident, and then with the passage of time it would fade away, until the next negative encounter.
Fortunately, in 1988 the Memphis Police Department had the foresight to develop at Crisis Invention Training (CIT) that included 40 hours with the goal of creating a jail diversion prior to arrest. Finally, a police officer who was under trained had a professional focus 40-hour quality training.
Adoption of CIT training across the country has been steady, but not ubiquitous. Being trained in CIT doesn’t guarantee the prevention of a negative outcome, but it does increase the chances of a positive outcome. Studies have shown CIT to be effective. The infrastructure supporting CIT has grown more professional each year. The future gets better as more CIT officers will be encountering these precarious situations.
Jail diversion and treatment is essential. An act of advocacy for those reading this article is to contact your local NAMI.org affiliate and inquire if the local police department has CIT training. If not, or if the percentage of officers trained is not 100% then ask how you can help. Contact your board of supervisors.
There have been so many recent news stories that have come to the conclusion that the criminal justice system has become the country’s answer to dealing with mental health that it is now common knowledge. CIT training is one piece of the solution puzzle for assisting this vulnerable population.
While many have claimed that the criminal justice system is the countries answer to mental health at this point, author German Lopez recently published an article examining the true ramifications of the claim. In the article, “How America’s Criminal Justice System Became the Country’s Mental Health System,” Lopez examines several cases where police officers have responded to deal with scenarios of mental illness.
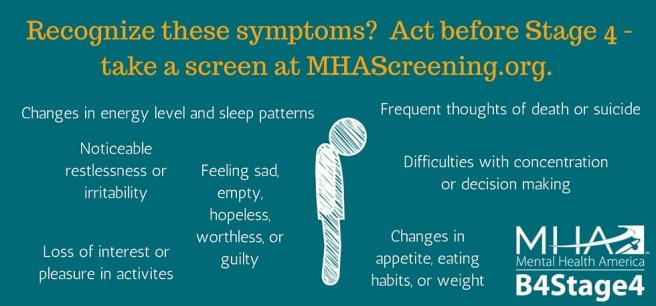
Officers respond to calls involving people who face both diagnosed and undiagnosed mental illnesses every day. It is important to remember what a police officer’s job is when they respond to such a call. When an officer arrives on scene, it is their job to uphold the law, and keep all citizens including themselves safe. Officers do go through extensive training to learn how to make these quick decisions, and what the best case scenario is. At the same time, the basic education they receive does not necessarily pertain to symptomatic mental illness.
When faced with someone who has decompensated and is in a state of complete mental breakdown, there is an immediate need for the officer to regain control to ensure that the person does not hurt themselves or anyone around them. In Lopez’s article, this critical moment in the decision making process is where one of two things occurs, either: “officers blasted him twice with a Taser, shocking him with 50,000 volts of electricity each time,” or “A police officer with training for mental health crisis, approached Kevin…this officer talked softly, reasoned with him, and finally, convinced him to get into the car-no violence necessary.” (vox.com.) Kevin is the same vulnerable person facing mental illness that went through both of these traumatic experiences.
The first experience of being tased, should not be the norm. It is the product of a cop making what they considered to be the best decision to regain control. Having a trained officer who responds to the situation with their voice rather than physical action, will go much further in that person’s recovery. Providing officers with education gives them knowledge about various illnesses, and how they may be evident in people’s behavior, as well as the best methods for making quick decisions on how to handle the situation. The proof of how well education works lies in the outcomes.
For Kevin, the person who went through both of the above encounters, it was because of the second officer’s communication and decision to take Kevin to the hospital that he was able to get help. He was able to fight the charges against him at the time, and best of all, “With proper care and medication, Kevin has not had a dangerous run-in with police in nearly 10 years since.” (vox.com) That right there speaks for itself. Kevin has been able to remain in control of himself through care and medication, and has not gotten violent to require police intervention in a decade.
There are thousands of Kevin’s out there, thousands of people who wind up in jail because of the disease they struggle with. These are people who courts deem unfit to stand trial, yet there is nowhere for them to go and not enough education out there to help police officers as they respond to the same call for the same person over and over again.
When a mentally ill person does commit crime, they are responsible. The solution is treatment before trouble. Through education, programs such as CIT, and the modern therapeutic treatment model, it is possible to allow police officers to do their job more effectively. By giving them knowledge of how to react to someone who is facing a mental illness, and providing them with tools and supports for where to take the person to get the best help, it is possible to reduce the chances of an immediate repeat situation and ultimately hopefully keep that person from entering the cycle of being in and out of jail.